A Q&A with Comagine Health 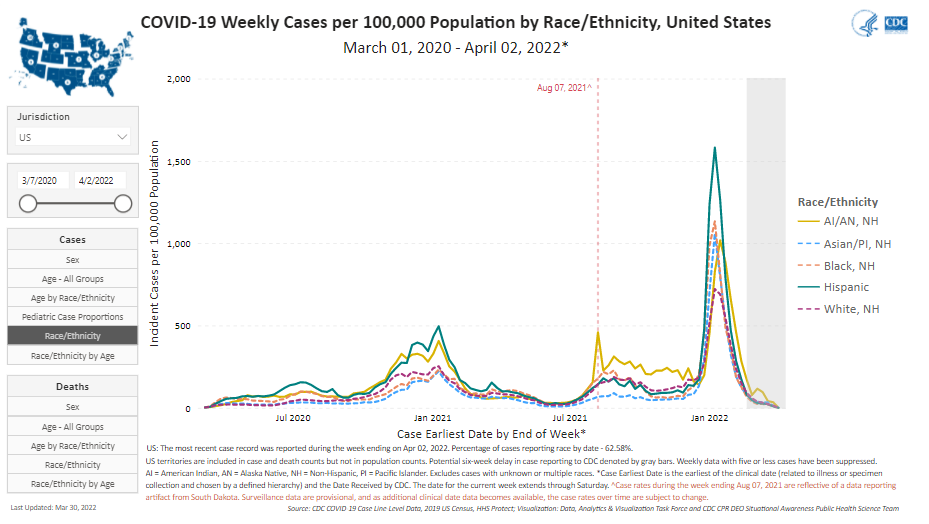
What has been the effect of the COVID-19 pandemic on the American Indian Alaska Native (AIAN) community?
The AIAN communities have been disproportionately impacted by the COVID-19 pandemic. Based on Centers for Disease Control and Prevention (CDC) data the AIAN population infection rates are over 3.5 times higher than non-Hispanic whites, AIAN individuals are over four times more likely to be hospitalized as a result of COVID-19, and the mortality among AIANs was 1.8 times that among non-Hispanic whites.
Nationally the indigenous population has one of the highest vaccination rates. The Indian Health Service (IHS) vaccination plan, including access and distribution, was very intentional to reach those hardest hit by the pandemic. IHS successfully implemented vaccination distribution and tracking that supplied facilities and tribes effectively, with the strict objective of no waste. The COVID-19 pandemic conditions brought attention to the native population, the living conditions, social determinants of health and the challenges in these communities.
The AIAN communities leaned on their cultural traditions and customs to respond to this pandemic and shared responsibility and care in their tribal communities. They rallied together to make a tragic situation one with valuable narratives of courage, community, and organizational success. This situation has also reinforced the public health role of tribes working together to fight the pandemic.
What are the biggest challenges of providers treating individuals in the AIAN community during the COVID-19 pandemic?
The providers had a heightened awareness of the importance in maintaining a trust relationship in caring for the AIAN community due to the underlying trauma of history and treatment of the indigenous community. The inability to control spread in overcrowded or multigenerational homes led to spread at a higher rate. Health care providers were faced with caring for multiple family members with COVID-19 as well as the mental health of other grieving family members.
A large issue has been inpatient bed capacity, both locally and outside in the referral facilities. When patients were discharged from outside facilities, they often still required medical supplies (e.g., oxygen) and heightened care. The lack of staffing and filled bed capacities in the rural hospitals meant that they could not admit the patients in many cases and supplies were not readily available. Additionally, the family had to transfer their relative back home; transport can often be a challenge in these communities.
The pandemic did result in some positive transformation as several facilities established or strengthened relationships with their community, state, and regional partners. These types of partnerships and collaboration helped the facilities to fill gaps, be more efficient, and maximize resources. Some facilities lacked the staffing and/or infrastructure to rapidly track, monitor, consistently report to the state, and assess community-level COVID data. In some areas with these conditions IHS granted the tribe public health authority to perform tracking and reporting at the community health representative level.
What are some of the strategies in the CMS approach to Quality that can make a lasting difference in promoting health equity in the AIAN community?
The entire AINHQI is about health equity! In terms of implementation strategies, the individual coaching and support we are providing at the local hospital-specific IHS level combined with the power of facilitated collaboration and learning across the 24 IHS hospitals and communities accelerates learning and promotes sustainability. IHS hospital clinicians, staff and leaders are building knowledge and skills and a long-term network of peer relationships and support as they address and promote health equity in their facilities and communities.
How has the focus of your Quality work changed during the pandemic, and how have your own professional experiences shaped those changes?
The pandemic and public health emergency have illuminated and exacerbated health disparities, including racial and ethnic disparities as well as geographic disparities. At the same time, the pandemic has elevated the need for a more comprehensive approach to quality which considers the whole person, the whole family, and the whole community. Each of us have experienced personal and professional tragedy and loss over the past two years, making us even more resolute about the essential nature of the quality work we do. The interconnectedness of health, safety and community is now at the forefront of our work and has helped us to focus on what matters and to measure and improve what matters. We are eager to further sharpen our support to IHS hospitals and tribal communities on leadership, organizational and personal resilience and culture, which are the building blocks necessary for quality and safety.
What advice would you give Quality Improvement professionals about promoting health equity?
Those of us who are quality professionals have long understood the need to put oneself in someone else’s shoes to be effective; that is, to go beyond the golden rule to the platinum rule – from “treat others how you would like to be treated” to “treat others how they would like to be treated.” Living the platinum rule has required respect and deep listening to drive and support lasting improvement. Now, as quality and health equity are so intertwined, we recognize the essential roles that self-awareness and trust play in our work as quality professionals. We each bring a multitude of identities and lived experience to our work in health care, and our work is grounded in relationships. As a result, committing to our own personal and professional journey of learning about ourselves, examining our implicit biases, and committing to fair and equitable care and treatment for all are the ways forward to be a trusted health professional colleague to those we are working with and ultimately to better care for and support patients, families and communities.
Submitted by Comagine Health.
This material was prepared by The Bizzell Group (Bizzell), the Data Validation and Administrative (DVA) contractor, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (HHS). Views expressed in this material do not necessarily reflect the official views or policy of CMS or HHS, and any reference to a specific product or entity herein does not constitute endorsement of that product or entity by CMS or HHS. 12SOW/Bizzell/DVA-1156-07/18/2023

