To protect Medicare beneficiaries and the Medicare Trust Fund, the Centers for Medicare & Medicaid Services (CMS) established Beneficiary and Family Centered Care-Quality Improvement Organizations (BFCC-QIOs). BFCC-QIOs help Medicare beneficiaries exercise their right to high-quality health care by providing assistance when beneficiaries have a concern about their care.
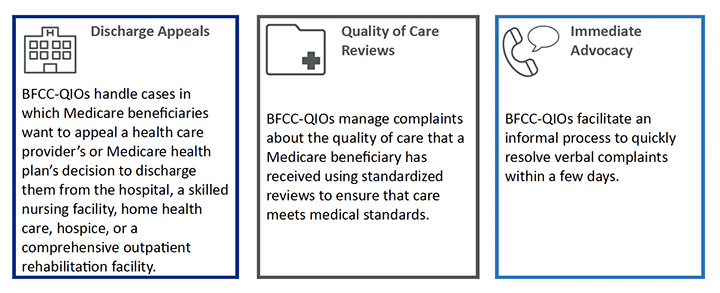
From June 2019 through April 2023, the BFCC-QIOs completed more than 1 million Discharge Appeal Reviews for Medicare beneficiaries, conducted almost 20,000 Quality of Care Reviews, and facilitated more than 40,000 Immediate Advocacy cases.
Support Services for Medicare Beneficiaries with a Focus on Timeliness
Understanding that coordination of healthcare services can be stressful and time-sensitive, the BFCC QIOs must complete case work within aggressive timelines. BFCC-QIO timeliness metrics ensure that beneficiaries and their families have the information they need for decision-making and next steps. In more than 95 percent of all cases, BFCC-QIOs met or exceeded their goals for timeliness and resolved cases for Medicare beneficiaries.
![]() Discharge appeals vary slightly by setting of care and whether the beneficiary is enrolled in Original Medicare or a Medicare Managed Care plan; after the BFCC-QIO has been notified of the appeal, the team has 24 to 72 hours to complete the appeal, depending on the setting and type of Medicare coverage.
Discharge appeals vary slightly by setting of care and whether the beneficiary is enrolled in Original Medicare or a Medicare Managed Care plan; after the BFCC-QIO has been notified of the appeal, the team has 24 to 72 hours to complete the appeal, depending on the setting and type of Medicare coverage.
In support of beneficiary-initiated Quality of Care complaints, BFCC-QIOs progress through a detailed set of steps to obtain input from the beneficiary or family member/representative about the nature of the complaint, obtain relevant medical records, review all files, and compare documentation of care delivered to current care standards. They then follow up with beneficiaries and providers or practitioners about the findings. At each step of the process, BFCC-QIOs maintain timeliness and ensure that documentation required for the review is available.
![]() Given the nature of Immediate Advocacy, which is intended to help resolve an issue or complaint in a collaborative and expedited fashion, these cases are typically resolved within two days of initiation. During this time, BFCC-QIOs help Medicare beneficiaries with communication problems between beneficiaries and their providers or practitioners for issues such as getting medical equipment or getting a prescription order sent to the pharmacy.
Given the nature of Immediate Advocacy, which is intended to help resolve an issue or complaint in a collaborative and expedited fashion, these cases are typically resolved within two days of initiation. During this time, BFCC-QIOs help Medicare beneficiaries with communication problems between beneficiaries and their providers or practitioners for issues such as getting medical equipment or getting a prescription order sent to the pharmacy.
Ensuring Services are Patient and Family Centered
In keeping with CMS’ commitment to deliver beneficiary and family-centered care, BFCC-QIOs have a mandate to ensure the support they provide is tailored for beneficiaries and results in a positive beneficiary experience.
 As part of beneficiary-initiated Quality of Care complaint reviews, BFCC-QIOs provide detailed and fact specific findings in a letter to Medicare beneficiaries. While the letter describes complex clinical content, using plain language helps beneficiaries understand the findings of the review and know what supports and next steps are available to them.
As part of beneficiary-initiated Quality of Care complaint reviews, BFCC-QIOs provide detailed and fact specific findings in a letter to Medicare beneficiaries. While the letter describes complex clinical content, using plain language helps beneficiaries understand the findings of the review and know what supports and next steps are available to them.
To ensure that BFCC-QIOs are delivering high quality, beneficiary-and family centered case review services, a sample of beneficiaries who received support from the BFCC-QIO are surveyed about their experience with the process. The survey asks about interactions with the BFCC-QIO, and support received through the process. Survey data provide ongoing feedback for BFCC-QIOs that help them implement quality improvement initiatives to deliver the best experience to Medicare beneficiaries and their families. In the most recent annual evaluation, 87 percent of surveys reflected a positive beneficiary experience with BFCC-QIO services.
Feedback from Medicare beneficiaries suggests the BFCC-QIOs are having the intended impact. One beneficiary who received support commented, “The people I interacted with were helpful with the steps, they got in contact with the facility, got back to me, explained that they would advocate and what steps I could take. I found them to be helpful. I had a good experience.”
The preparation of this publication was performed under Contract No. 75FCMC19D0068 75CMC19F0001, funded by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services and/or CMS nor does mention of organizations imply endorsement by the U.S. government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
Stephanie Fry is the Deputy Project Director with the BFCC NCORC.
Sandra Zelaya is a Communications Specialist with the BFCC NCORC.
The authors declare no conflicts of interest.
Address for correspondence: Wendy Gary, Avar Consulting, Inc. 1395 Piccard Drive, Suite 200 Rockville, MD 20850. (wgary@avarconsulting.com). Publication Number: ACD-2023-NCORC-0251

