A Missouri hospital teamed with Health Quality Innovators (HQI), a Centers for Medicare & Medicaid Services (CMS) Hospital Quality Improvement Contractor (HQIC), to successfully decrease its readmission rates. As a part of this partnership, HQI and the hospital identified factors that contribute to readmissions and set out to tackle a root cause.
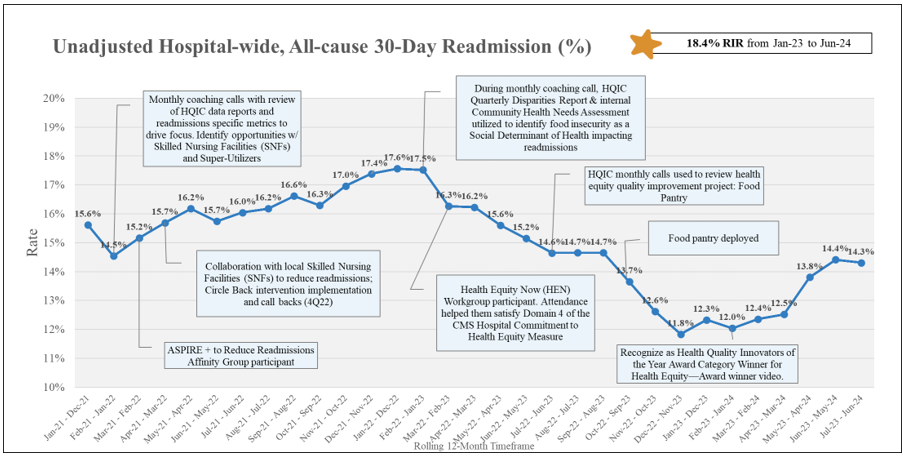
The acute care hospital in Southeast Missouri is situated in an area with high socioeconomic factors that impact patients. As a result of collaborating with HQI, the hospital achieved an 18.4 percent Unadjusted Hospital-wide All-cause 30-day Readmission Relative Improvement rate (RIR) between January 2023 and June 2024. Figure 1 below illustrates the hospital’s progress in reducing their readmission rate during this timeframe.
Figure 1. Unadjusted Hospital-wide, All-cause 30-day Readmission
Using Data to Identify Social Determinant Need
Monthly coaching calls and data analysis provided by the HQI Quality Improvement Advisor helped the hospital target their initial interventions on reducing readmissions for multi-visit patients and readmissions from skilled nursing facilities.
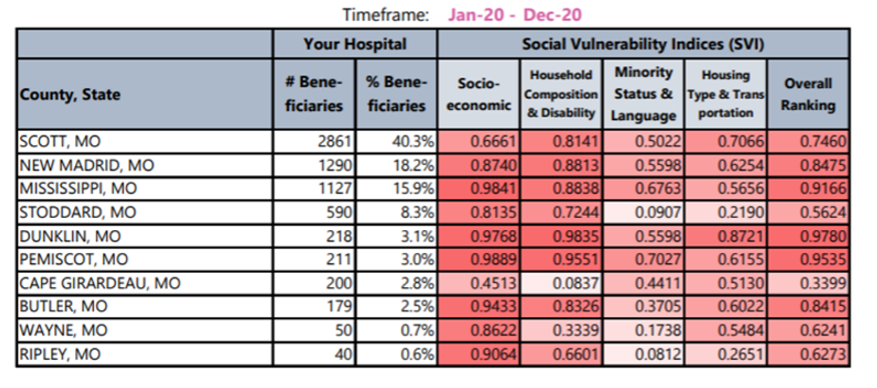
The hospital used Community Health Needs Assessment (CHNA) data and the Social Vulnerability Indices (SVI) within the HQIC Quarterly Disparities report provided by HQI, to identify food insecurity as an issue impacting their patient population.
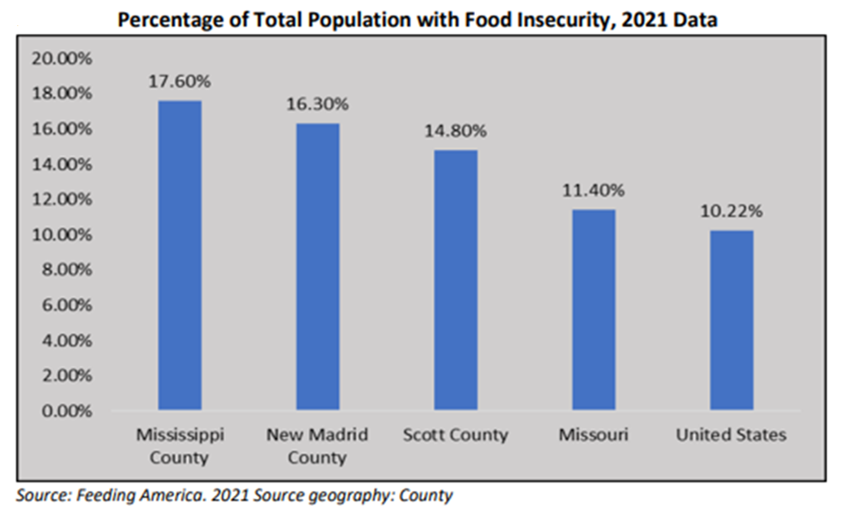
In Figure 2 below, the CHNA highlighted the percentage of the total population that experienced food insecurity. Counties served by the hospital were higher than the national average.
Figure 2. Percentage of Total Population with Food Insecurity (2021) Data
HQI provided a Quarterly Disparities Report (Table 1) to highlight socioeconomic concerns. The report showed that the majority of counties served by the hospital ranked as having ‘high to very high’ levels of socioeconomic issues. The SVI values range from 0 (least vulnerable) to 1 (most vulnerable). SVI is categorized as follows: Very Low (0.0-0.19); Low (0.20-0.39); Moderate (0.40-0.59); High (0.60-0.79); Very High (0.80-1.0).
Table 1. Quarterly Disparities Report
 Identifying Patients Who Have Food Insecurity
Identifying Patients Who Have Food Insecurity
In working with the hospital, HQI proposed using the Plan-Do-Study-Act (PDSA) methodology. To determine the needs of specific patients, the hospital’s social services used the Protocol for Responding to and Assessing Patients' Assets, Risks and Experiences (PRAPARE) screening tool which included the following questions.
- In the last 12 months, have you not been able to purchase food? (Y/N) _________
- In the last 12 months, have you been living paycheck to paycheck wondering if you could afford food? (Y/N) __________
- If “yes” to either question above:
- Are you agreeable to having the Food Pantry contact you and you can be discharged with 20 lbs. of food?
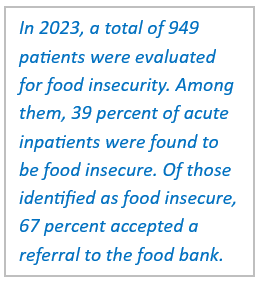
If the patient was identified by Social Services or Case Management as having food insecurity, the hospital provided them with food and sent a referral to a food bank. If the patient identified having any other needs, they were given a list of additional resources. With a solid framework in place, the hospital set a goal of reducing the number of patients identified as having food insecurity by 10 percent within the next three years by implementing a patient food pantry at the hospital.
Participation in HQI’s Health Equity Now (HEN) Learning Series
In addition to coaching calls and helping with data analysis, HQI invited the hospital to participate in the Health Equity Now (HEN) series, HQI's six-month workgroup that assisted hospitals in designing, implementing and maintaining health equity programs. Participants met twice a month in learning sessions that featured lectures on best practices and recommendations. Health Equity Huddle Sessions offered participants opportunities to collaborate with peers. One of the focuses of the workgroup was addressing disparities in readmissions.
As a result of best practices learned by participating in the HEN series, the hospital implemented the following strategies.
Developed a hospital committee focused on the food pantry initiative. Committee members included representatives from the Population Health Department, Social Services, Case Management/Quality, Marketing and the hospital Foundation. A dietary director provided assistance in locating on-site storage for food to stock the pantry.
Informed patients of call backs. When food is brought to the patient before discharge, Social Services staff use this opportunity to remind patients about the upcoming call they would receive from the hospital. This reminder led to more successful follow-up calls to ensure that patients had scheduled appointments, filled prescriptions and understood discharge instructions.
Partnered with local food bank to provide additional assistance to patients when they are discharged from the hospital. Individuals are connected to other food assistance services in the community, such as food banks, a monthly senior food box service or help applying for Supplemental Nutrition Assistance Program (SNAP) benefits.
Keys to Success
HQI’s success can be replicated by taking the following steps:
- Utilize multiple data sources such as the CHNA and SVI data to identify patient needs.
- Assess the social needs of patients during their hospital stay and connect them with appropriate resources.
- Build sustainable community partnerships with organizations to address patient needs long-term.
This hospital was recognized as the winner of the 2023 Health Quality Innovators of the Year Award for their efforts in health equity. Learn more about their food pantry initiative by viewing the hospital’s category winner video.
For more information, visit HQI.solutions.
This material was prepared by The Bizzell Group (Bizzell), the Data Validation and Administrative (DVA) contractor, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (HHS). Views expressed in this material do not necessarily reflect the official views or policy of CMS or HHS, and any reference to a specific product or entity herein does not constitute endorsement of that product or entity by CMS or HHS. 12SOW/Bizzell/DVA-1423-07/31/24

