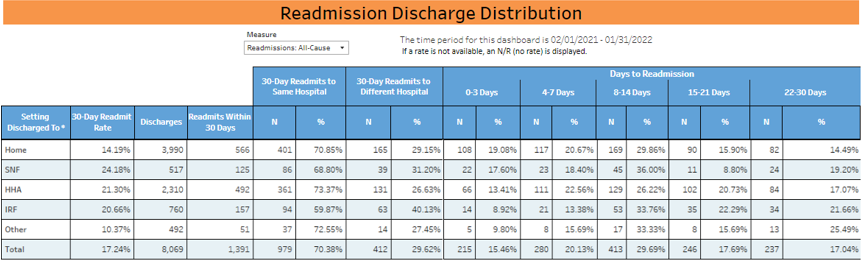
Health Services Advisory Group (HSAG), a Centers for Medicare & Medicaid Services (CMS) Hospital Quality Improvement Contractor (HQIC), is dedicated to a data-driven process to strategically target readmission areas that have the greatest opportunity for improvement. Leveraging the HSAG HQIC Quality Improvement Innovation Portal (QIIP) performance dashboard (Figure 1), hospitals can see their readmission rates per discharge setting, the number of readmissions within 30 days, whether the readmission was to the same or a different hospital, and the number of days to readmission. HSAG HQIC quality advisors (QAs) are then able to assist hospitals in identifying trends in readmission diagnoses, discharge disposition and other key factors in implementing targeted, data-driven interventions and strategies.
Using Data to Facilitate Collaboration and Reduce Readmissions
For example, one hospital leveraged HSAG QIIP performance dashboard data to facilitate collaboration and engagement with community home health providers related to increased readmissions. The hospital stated that the aggregate readmission discharge distribution data HSAG HQIC provided in the performance dashboard helped the hospital identify a concerning trend with a higher proportion of readmissions coming from home health agencies (HHAs), compared with other settings. Based on this finding, the hospital is working with HHAs to conduct a root cause analysis into why readmissions from HHAs are so high. HSAG HQIC deploys the 7-Day Readmission Chart Audit Tool. This allows hospitals to fine-tune their discharge and care transitions process.
Engaging Patients, Families and Caregivers
Another critical component to addressing readmissions is engaging patients, families and caregivers. HSAG HQIC created several Zone Tools to assist in post-discharge self-management of conditions. Hospitals use Zone Tools to engage patients and families to participate in care, monitor chronic conditions and provide guidance on when to call the health care team when changes in conditions occur. The tools can be used regardless of the discharge disposition. As hospitals implement these interventions, HSAG HQIC continues to provide technical assistance to hospitals through routine coaching calls.
Figure 1. Readmission Discharge Distribution
Identifying Disparities in Readmissions
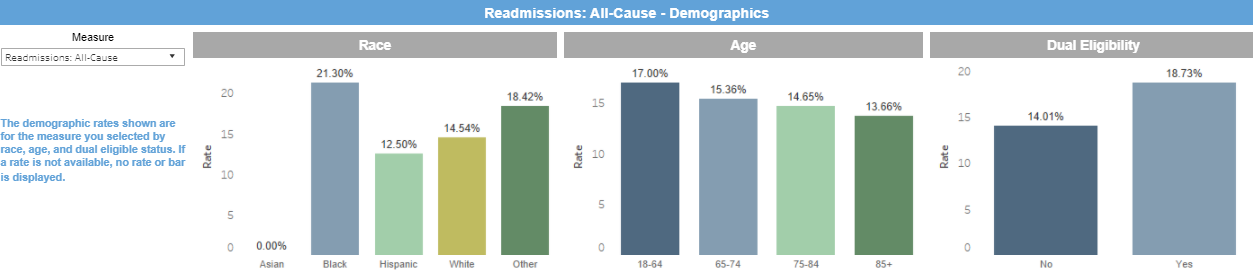
HSAG HQIC also focuses on assisting hospitals in identifying disparities in readmissions by leveraging the demographics section of the QIIP performance dashboard. For example, Figure 2 below shows 30-day readmission rates by race, age and dual eligibility status for one hospital. The graph shows that, compared to individuals who are white, those who are black are more likely to be readmitted to the hospital within 30 days, and individuals who have both Medicare and Medicaid (dual eligibility) are more likely to be readmitted than non-dual eligibles.
The dual eligibility status is being used as a proxy measure to identify potential social determinants of health (SDOH) that affect readmission rates. HSAG HQIC QAs provide technical assistance to hospitals to implement interventions to target specific disparities. For example, the HSAG HQIC Social Work Assessment assists hospitals in identifying socioeconomic needs for patients prior to discharge. This is especially important for high utilizers and patients from catchment areas with high Area Deprivation Index scores.
Figure 2. Readmissions: All-Cause Demographics by Race, Age and Dual Eligibility
For more information, visit https://www.hsag.com/en/hqic.
This material was prepared by The Bizzell Group (Bizzell), the Data Validation and Administrative (DVA) contractor, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (HHS). Views expressed in this material do not necessarily reflect the official views or policy of CMS or HHS, and any reference to a specific product or entity herein does not constitute endorsement of that product or entity by CMS or HHS. 12SOW/Bizzell/DVA-1157-07/18/2023

