
A New Hampshire (NH) hospital successfully reduced anticoagulation-associated adverse drug events (ADEs) in partnership with The Healthcare Association of New York State (HANYS), a Centers for Medicare & Medicaid Services (CMS) Hospital Quality Improvement Contractor (HQIC); the New Hampshire Hospital Association (NHHA) and the Foundation for Healthy Communities (FHC). From March 2021 to July 2023, the hospital had 15 incidents of anticoagulation-associated ADEs. During post-intervention from August 1, 2023, through February 29, 2024, the hospital had no incidents of anticoagulation-associated ADEs.
The Eastern U.S. Quality Improvement Collaborative, known as EQIC, was established in 2020 by HANYS to deliver services for the CMS HQIC contract to further advance the quality and safety of health care provided in hospitals. The NH EQIC Project Manager as well as EQIC partners, NHHA and FHC, shared data, tools and resources with the hospital. The project manager also encouraged the hospital to participate in webinars and the ADE affinity group for peer networking, best practice sharing, data review and action planning.
Aligning Pharmacy Anticoagulation Management Process
The hospital is part of a larger health system comprised of five hospitals and multiple clinics and operates under a continuous quality improvement model. This includes monitoring medications for ways to improve the facility’s medication use process. The NH EQIC Project Manager routinely meets with the quality leaders at the hospital to review outcome data and discuss ongoing quality improvement projects. In 2019, the hospital recognized the need to align their anticoagulant protocols in their electronic health record (EHR) across the health care system. It was discovered that each facility within the hospital system used varying protocols for administrating heparin, a type of anticoagulant. Some hospitals relied on nurses to perform manual calculations when making infusion rate adjustments, so hospital staff were dosing and following slightly different monitoring frequencies and parameters.
The hospital formed a large system committee and a pharmacist-led anticoagulation subcommittee that focused on aligning pharmacy and therapeutics in the EHR. Committee members included pharmacists, cardiologists, hematologists, hospitalists, nurses and information technology (IT) specialists. Hospitalists were important to include on the committee, as they serve as the quarterback of the hospital – having experience serving all patient types. IT specialists were vital to incorporate workflows into the EHR. Pharmacists assisted as liaisons to align anticoagulation management across facilities. As a result, the hospital aligned pharmacists throughout their facilities under one group to standardize anticoagulation management processes across hospitals.
Interventions Identified to Decrease Anticoagulant ADEs
With the help of the HANYS HQIC team, the hospital reduced its anticoagulation-associated ADEs by implementing the following interventions:
- Aligning a pharmacy anticoagulation management process to improve patient care.
- Updating heparin infusion management with changes to weight-based calculations for rate adjustments.
- Adopting new oral anticoagulants (NOACs) over warfarin for long-term anticoagulation in atrial fibrillation and venous thromboembolism cases.
- Developing an anticoagulation stewardship scoring tool to improve monitoring efficiency and identify potential gaps.
Updating Heparin Infusion Management
The hospital changed their heparin infusion protocols in their EHR using patient data, such as weight, to better tailor dosage to each patient. They reduced the number of order sets to four, making them more indication-specific, aligning order sets with specific indicators to make it easier for providers to select the most appropriate order set based on medical necessity. These processes decreased the need for nurses to perform calculations when making infusion rate adjustments. By monitoring this process through data collected from the EHR, the hospital noted a decrease in the number of patient adjustments that needed to be made after a patient was put on an anticoagulant.
Adopting New Oral Anticoagulants (NOACs) Over Warfarin
The use of NOACs for chronic oral anticoagulation also contributed to the success of reducing anticoagulant ADEs. This change was driven by updates to national practice guidelines, that recommend NOACs as a first-line therapy over warfarin.
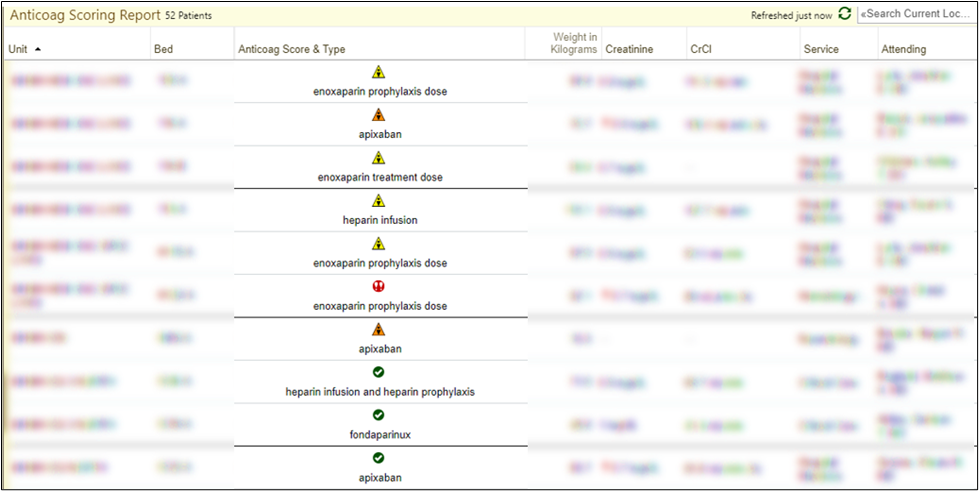
Developing an Anticoagulation Stewardship Scoring Tool
A scoring tool (Figure 1.) comprised of guidelines designed to pinpoint risk factors associated with anticoagulant utilization such as hypertension or diabetes, was developed to improve monitoring and identify potential gaps in patient care. These guidelines may flag instances of dosage discrepancy relative to indication, identify worrisome trends in laboratory values warranting dosage adjustments, or highlight a heightened risk of adverse events. The guidelines are integrated into the EHR, where a patient’s medical record is systematically reviewed for these specified data points. If the data aligns, a rule is triggered, and a score is generated that creates a checklist for a pharmacist to complete a first review of anticoagulant therapies. If an opportunity is identified to optimize the patient's care, the pharmacist alerts the patient's provider team and works with them to make changes. The hospital is in the process of implementing the scoring tool across pharmacies through their EHR.
Figure 1. Stewardship Scoring Tool
Keys to Success
The hospital’s success reducing anticoagulation-associated ADEs can be replicated by taking the following steps:
- Align pharmacy procedures in facilities across the health care system to provide efficient, quality care to Medicare patients.
- Develop necessary tools to efficiently and accurately monitor ADEs associated with anticoagulation medications.
- Leverage the expertise of analysts to ensure protocols are functioning as intended within an EHR.
For more information, visit HANYS and Eastern US Quality Improvement Collaborative (EQIC).
This material was prepared by The Bizzell Group (Bizzell), the Data Validation and Administrative (DVA) contractor, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (HHS). Views expressed in this material do not necessarily reflect the official views or policy of CMS or HHS, and any reference to a specific product or entity herein does not constitute endorsement of that product or entity by CMS or HHS. 12SOW/Bizzell/DVA-1383-06/06/24

