The Centers for Medicare & Medicaid Services (CMS) Quality Improvement Organization (QIO) Program is dedicated to improving health care quality at the community level. Hospital Quality Improvement Contractors (HQICs) are strategic partners of the QIO Program dedicated to improving the quality of care delivered to people with Medicare in hospitals.
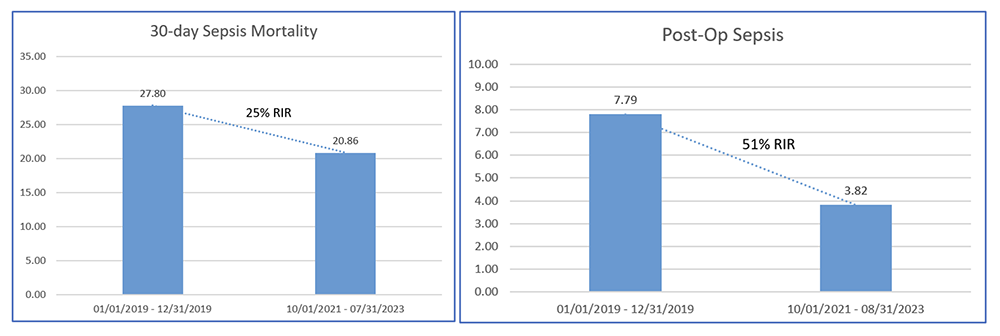
Through its role as an HQIC, TMF Health Quality Institute (TMF) and the Arkansas Hospital Association, partnered with a large Arkansas hospital to decrease its sepsis rate. Working with TMF, the hospital achieved a 25 percent Relative Improvement Rate (RIR) in sepsis mortality between January 2019 and July 2023 and a 51 percent RIR for post-op sepsis achieved between January 2019 and August 2023.
The hospital completed a mortality analysis and a Patient Safety Indicator 90 (PSI90) analysis, which identified an opportunity for the septic population. The hospital cross-functional team identified sepsis for documentation and coding improvements due to its high volume. TMF worked with the hospital’s quality improvement point of contact and provided their Process Improvement Discovery Tool to assist the hospital in identifying process improvement opportunities for reducing cases of sepsis. TMF’s Sepsis Mortality Reduction Top Ten Checklist was also provided to assist in reviewing current interventions or initiating new ones, to reduce sepsis mortality. The Process Improvement Discovery Tool (Post-op Sepsis Prevention Process) was shared to identify improvement opportunities for post-op sepsis prevention. To address the opportunities for improvement, the hospital and TMF identified the following interventions:
- Improve communication between hospital staff about sepsis cases
- Develop logic in EHR to identify sepsis cases
- Implement physician-to-physician education
Improve communication between hospital staff about sepsis cases
Support from senior-level hospital executives and the hospital medical board was key to adopting sepsis as an institutional priority and achieving its goals. Senior leaders were very involved in priority and goal setting. They sponsored the work, attended regular meetings and made sure any barriers were removed. Additionally, hospital leaders spoke at the hospital medical board and QUEST (the hospital’s quality, experience, safety oversight committee) about the importance of working to decrease sepsis, the sepsis pathway, and the communication exchange expected between physicians and nurses regarding patients’ septic status. To reinforce messaging, emails were sent to all residents and physicians, and unit managers were responsible for educating bedside nurses.
One key component of improving communication between hospital staff was the implementation of a no-harm approach to identifying sepsis patients. If the emergency department (ED) called for a hospital consult for a possible sepsis case and it turned out that the patient did not have sepsis, this was not frowned upon. The hospital’s approach is that there is “no harm” in calling a physician to evaluate a patient. Like the Preoccupation with Failure principle in a High-Reliability Organization (HRO), employees are encouraged to report their concerns about potential failures. This no-harm approach eliminated hesitation for hospital staff to alert physicians of a patient with possible sepsis. The hospital quality department also played a key role by sharing data with members of a management guidance team made up of representatives from medical and surgical specialties, quality, billing, coding and nursing.
Develop logic in the EHR to identify sepsis cases
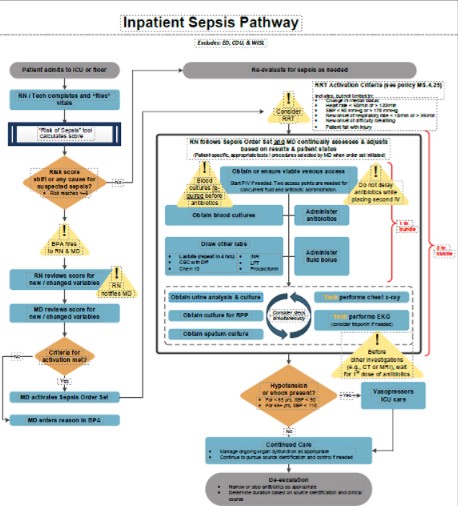
The management guidance team worked together to develop a sepsis protocol referred to as the Inpatient Sepsis Pathway. This protocol set the foundational work that allowed for infectious disease physicians and nurse leaders to be notified of sepsis cases to provide treatment.
To make it easy for staff to comply with the new sepsis protocol, the hospital hardwired alerts and bundled orders into its Electronic Health Record (EHR). The hospital’s EHR Inpatient Sepsis Pathway is used to screen patients, which begins calculating at admission. Once a patient reaches a certain score, a best practice alert (BPA) is sent to both the infectious disease nurse and the physician. As a result, the nurse contacts the physician, and the physician follows the sepsis order set or justifies why the order set is not needed.
Implement physician-to-physician education
In addition to the alerts and order sets hardwired into the EHR, the hospital implemented physician-to-physician education about the need to order lactate labs and repeat labs when needed. Education was provided in grand rounds and resident systems conferences. TMF’s Sepsis Mortality Reduction Top Ten Checklist was given to attending physicians and training physicians.
Keys to Success
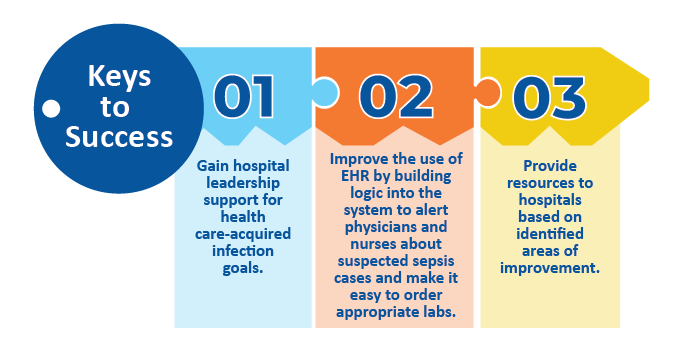
TMF’s success can be replicated by taking the following steps:
- Gain hospital leadership support for health care-acquired infection goals.
- Improve the use of EHR by building logic into the system to alert physicians and nurses about suspected sepsis cases and make it easy to order appropriate labs.
- Provide resources to hospitals based on identified areas of improvement.
For more information, visit tmfnetworks.org.
This material was prepared by The Bizzell Group (Bizzell), the Data Validation and Administrative (DVA) contractor, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services (HHS). Views expressed in this material do not necessarily reflect the official views or policy of CMS or HHS, and any reference to a specific product or entity herein does not constitute endorsement of that product or entity by CMS or HHS. 12SOW/Bizzell/DVA-1267-12/22/23

